A University of Guelph professor and internationally-renowned chemist has had four of his vaccine candidates for bacterial infections recognized by the World Health Organization.
The report, which aims at increasing understanding and investment in research into what they call a "hidden pandemic," is their first analysis of bacterial vaccines in preclinical development and human trials that are being developed to treat “priority pathogens,” antibiotic-resistant bacteria that “pose the greatest risk to human health."
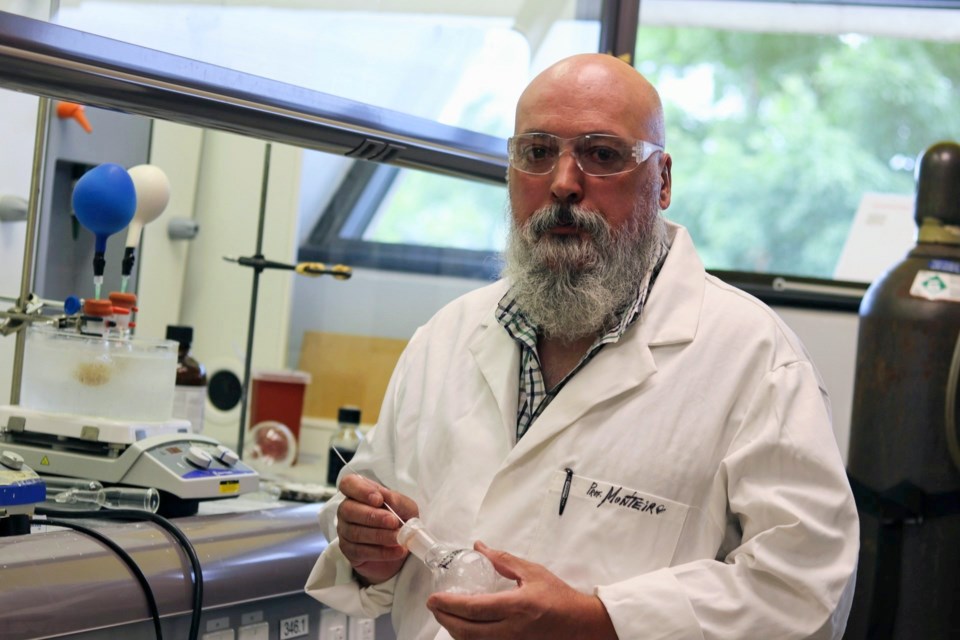
“People overuse antibiotics. The problem with viruses is that it might be viral now, but your immune system crashes a bit and then the bacteria goes in,” said professor Mario Monteiro.
The four vaccines listed from Monteiro are for diarrhea – primarily travellers diarrhea – caused by campylobacter, C. difficile, E. coli and shigella bacterial infections.
Antibiotic-resistant bacteria like these cause around five million deaths worldwide in 2019. If left untreated, they could cause nearly2.5 million deaths in North America, Europe and Australia by 2050, and even more in developing nations.
Campylobacter, the most common bacterial cause of diarrhea, belongs to the foodborne pathogens like raw chicken, which is why you have to cook your meat well.
“Chicken carries a lot of campylobacter as a normal thing, doesn't bother the chickens. But if you eat raw chicken, it's got campylobacter, you get diarrhea,” he said.
Two of his vaccines listed treat campylobacter, one of which is in its second human trials.
Monteiro began researching a vaccine for it after being approached by the U.S. Navy 20 years ago, “because as you can imagine, soldiers are a specific type of traveller. They leave their base, they get diarrhea. So it's a big deal for the Navy.”
Twenty years might seem like a long time, but vaccines like these take decades to make in an academic setting. Even after entering human trials, the campylobacter vaccine is at least six years away from being released.
Although development is not as far along, he believes his C. difficile vaccine will be the most impactful of the four.
A few years back, he was reading the newspaper in the university centre, when he read an article about an antibiotic resistant C. difficile outbreak somewhere, a germ that causes diarrhea and colitis.
“Diarrhea? I go ‘well, this is up my alley, right?’”
When he found there was nothing known about the sugars on the bacteria, he began working on a vaccine.
While the germ naturally found in most people, it doesn’t cause harm until you take antibiotics, which kill off both good and bad bacteria, allowing C. diff to take over.
“That's probably going to be the most impactful because (with) campylobacter, you'll get diarrhea, but you don't see anybody dying on the street because of it. But C. diff, you go to the hospital. It's a big deal,” he said.
In 2017, it was licensed by a U.S. biotech company, and is one of five C. diff candidates in preclinical development listed by the WHO.
The fourth vaccine listed in the report is a three-in-one vaccine, also funded by the U.S. Navy, treating campylobacter, E. coli and shigella infections. All three cause diarrhea, but the latter is typically accompanied by fever and stomach cramps, and is especially dangerous for children.
“It's actually one of the preferred products to use in the developing world, because then instead of just buying one dose of one bacteria, you buy one (vaccine) to target three bacteria.”
While most vaccine candidates focus on bacterial proteins, his campylobacter and C. diff vaccines are sugar-based.
His research team – currently made up of two students, Patricia Pham and Nolan Frame – is one of the few in the world that works to determine the sugars on the bacteria surface, called polysaccharides.
For instance, spike proteins, like those found on the surface of the virus that causes COVID-19, is a glycoprotein, meaning it has sugar surrounding it.
“When the virus and the RNA vaccine goes into your cells and makes the spike protein, your genes put sugars on it to fool your immune system,” he said.
The sugars are the first thing, along with the proteins, on the surface of the bacteria that your immune system recognizes when you get infected.
So they extract the sugars from the molecule, tweak it a bit to make it more immunogenic by linking it with protein that creates a strong immune response, and inject that into the vaccine. Your immune system will then make antibodies against the sugars of the bacteria, and will be able to recognize them if you ever become infected.
Determining what sugars exist on the bacteria surface is the first step of creating the vaccine, which alone can take years to do.
Fortunately, Monteiro said being listed in the report could potentially increase the amount of interest in his research, which could lead to more funding and research opportunities.
You can read the full report here.